Background
During neonatal resuscitation, supplemental oxygen is titrated to achieve targeted oxygen saturation (SpO2) values for the first ten minutes of life as specified by the Neonatal Resuscitation Program (NRP) guidelines. However, this is challenging for healthcare providers as they need to compare a constantly changing data stream (SpO2) with a paper cognitive aid for the appropriate SpO2 ranges over time while resuscitating a neonate in the delivery room.
Objective
To determine how the introduction of a data display with appropriate SpO2 ranges affects visual attention and decision-making of resuscitation team leaders for oxygen supplementation performance during simulated neonatal resuscitation.
Methods
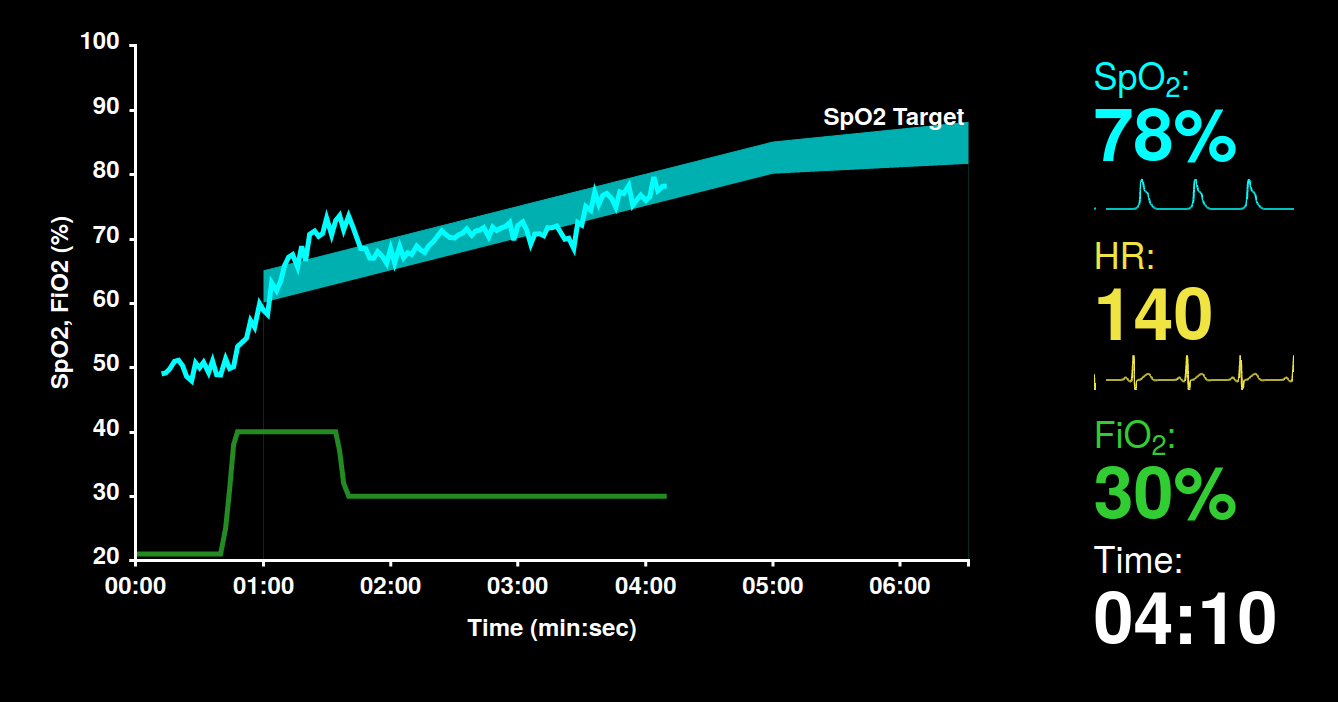
We compared a standard vital signs display and a novel display with our visual SpO2 targeting system based on NRP targets in a crossover study (n=22) with NRP card carrying healthcare providers. Subjects acted as team leader during two pairs of standardized resuscitation scenarios of fixed duration (easy and challenging). For each pair of scenarios, one scenario used the standard display, while the other scenario used the novel display; the order of displays was randomized for each scenario pair and each participant. Subjects wore an eye tracking system to record their gaze pattern and fixations, and all intervention decision events and simulated vital signs were logged.
Results
For easy scenarios, the two displays did not produce significant differences in decision-making performance outcomes. For difficult scenarios, the two displays did not produce a significant difference in duration of SpO2 maintenance near NRP targets. However, stratifying subjects by whether they had led at least one resuscitation in labor and delivery in the past year revealed that subjects with such recent practice were able to maintain SpO2 within NRP targets for significantly longer on the easy scenarios with the display than without [25 s; p-value 0.015]. With the novel display, subjects spent significantly more time looking at SpO2-related display elements [11 s; p-value 0.007]. On easy scenarios, subjects with recent practice leading resuscitation in labor and delivery showed additional differences in visual attention not found in other combinations of subject group and scenario-difficulty, including less time looking at the infant [17 s; p-value 0.024], more time looking at the monitor [20 s; p-value 0.019], and less time looking at the Apgar timer on the monitor [9 s; p-value 0.018].
Conclusions
Introducing a novel visual SpO2 targeting system may not by itself improve decision-making performance for oxygen supplementation. Rather, other factors such as prior experience and training may be strong determinants of the benefit of such a system. Furthermore, visual attention behaviors with such displays differ significantly based on prior experience and cognitive workload.